Background: In patients with chemo-sensitive relapsed diffuse large B-cell lymphoma (DLBCL), autologous hematopoietic cell transplant (ASCT) has long been the standard of care. Several recent studies have identified patient groups with poor post-transplant outcomes and in recent years chimeric antigen receptor (CAR)-T therapy has been utilized in patients who do not have adequate disease control to proceed with ASCT or who progress after ASCT. We hypothesized that the availability of CART to treat patients with aggressive lymphoma who were not ideal candidates for ASCT would lead to improved survival among lymphoma patients proceeding to transplant. We evaluated whether the demographics, baseline characteristics and post-ASCT outcomes for patients with relapsed non-Hodgkin lymphoma (NHL) have changed in the CAR-T era.
Methods: We included patients initially diagnosed with DLBCL since 2012 who subsequently relapsed and received ASCT. Patients who completed ASCT without a documented relapse or who received CART therapy prior to an ASCT were excluded as were patients without adequate follow-up data. Patients who completed ASCT prior to January 1, 2018, were part of the pre-CART group while those completing ASCT on January 1, 2018 and later were part of the post-CART group. We compared demographics as well as disease and treatment-related variables of interest between the pre- and post-CART groups using Fisher's Exact or chi Square tests as appropriate for categorical and ANOVA for numeric variables. In addition, we determined progression-free (PFS) and overall survival (OS) from the date of ASCT using the Kaplan-Meier method and determined predictors of post-ASCT PFS and OS using the Cox Proportional Hazards model with backward elimination.
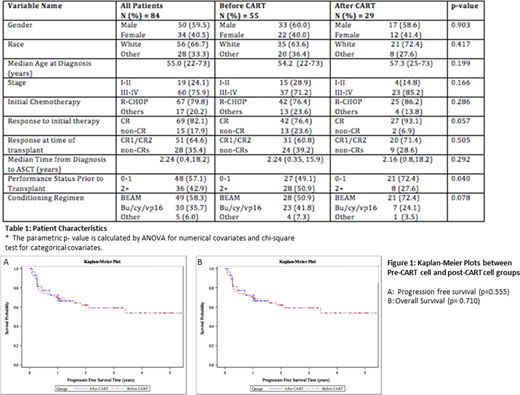
Results: Of 84 included patients, 55 were in the pre-CART group and 29 were in the post-CART group. Median age at diagnosis for all patients was 55 years (range 22-73). 50 were male, and 60 had stage 3 or 4 disease. While there were no differences in demographics based on treatment group, the ECOG performance status for patients in the post-CART group was improved compared to those pre-CART (Table 1, p=0.040). There was also no difference in time from diagnosis to transplant between the two groups (Table 1, p=0.292). With a median follow-up post ASCT of 2.22 years for the pre-CART group and 1.24 years for the post-CART group, the median OS was 4.7 years (95% CI: 3.4 - Not Reached) for the entire cohort, 4.7 years (95% CI: 2.8 - Not Reached) for the pre-CART group and not reached (95% CI: NR-NR) for the post-CART group. The median PFS was not reached in either cohort (p=0.932). Neither univariate nor multivariable analysis showed any of covariates as being significant predictors of post-ASCT PFS. In the multivariable model for OS, receiving R-CHOP chemotherapy compared to other induction regimens (HR 0.28 [0.10-0.74], p=0.01) predicted improved OS while increased age (HR 1.06 [1.01-1.11], p=0.03) predicted inferior OS. The receipt of ASCT after CART cell era, conditioning regimen, or first salvage regimen all did not impact PFS or OS.
Conclusion: In comparison with those patients receiving autologous transplantation prior to the adoption of CAR T cell, patients receiving ASCT more recently had no change PFS or OS despite having better performance status prior to ASCT. Our findings suggest that selection of appropriate candidates for ASCT in the current era is critical and that patients who are at higher risk for early post-ASCT relapse should be considered for novel approaches including immune effector cell therapy. Additional follow-up will be needed to determine if newer currently approved therapies for post-ASCT relapse can improve OS in relapsed/refractory DLBCL who relapse after ASCT.
Waller:Verastem Oncology, Inc: Consultancy, Research Funding. Allen:Curio Sciences: Honoraria; Bayer: Consultancy, Other; Clinical Care Options: Speakers Bureau; Research to Practice: Speakers Bureau; Imbrium: Consultancy, Other. Lonial:JUNO Therapeutics: Consultancy; Amgen: Consultancy, Honoraria, Other: Personal fees; Abbvie: Consultancy; Sanofi: Consultancy; Karyopharm: Consultancy; Genentech: Consultancy; Onyx: Honoraria; Janssen: Consultancy, Honoraria, Other: Personal fees, Research Funding; Takeda: Consultancy, Other: Personal fees, Research Funding; Novartis: Consultancy, Honoraria, Other: Personal fees; BMS: Consultancy, Honoraria, Other: Personal fees, Research Funding; GSK: Consultancy, Honoraria, Other: Personal fees; Merck: Consultancy, Honoraria, Other: Personal fees; Millennium: Consultancy, Honoraria; TG Therapeutics: Membership on an entity's Board of Directors or advisory committees. Kaufman:Tecnopharma: Consultancy, Honoraria; Janssen: Consultancy, Honoraria; Karyopharm: Membership on an entity's Board of Directors or advisory committees; Pharmacyclics: Membership on an entity's Board of Directors or advisory committees; Incyte: Consultancy, Membership on an entity's Board of Directors or advisory committees; Takeda: Consultancy, Honoraria; Celgene: Consultancy, Honoraria; Bristol-Myers Squibb: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; AbbVie: Consultancy; TG Therapeutics: Consultancy, Membership on an entity's Board of Directors or advisory committees; Sanofi/Genyzme: Consultancy, Honoraria. Hofmeister:Janssen: Honoraria, Research Funding; Oncolytics Biotech: Research Funding; Imbrium: Honoraria; Oncopeptides: Honoraria; Bristol Myers Squibb: Honoraria, Research Funding; Nektar: Honoraria, Research Funding; Sanofi: Honoraria, Research Funding; Karyopharm: Honoraria, Research Funding. Dhodapkar:Janssen: Membership on an entity's Board of Directors or advisory committees, Other; Kite: Membership on an entity's Board of Directors or advisory committees, Other; Lava Therapeutics: Membership on an entity's Board of Directors or advisory committees, Other; Celgene/BMS: Membership on an entity's Board of Directors or advisory committees, Other; Amgen: Membership on an entity's Board of Directors or advisory committees, Other; Roche/Genentech: Membership on an entity's Board of Directors or advisory committees, Other. Nooka:Oncopeptides: Consultancy, Honoraria; Spectrum Pharmaceuticals: Consultancy; Celgene: Consultancy, Honoraria, Research Funding; Sanofi: Consultancy, Honoraria; Adaptive Technologies: Consultancy, Honoraria; Karyopharm Therapeutics, Adaptive technologies: Consultancy, Honoraria, Research Funding; GlaxoSmithKline: Consultancy, Honoraria, Other: Personal Fees: Travel/accomodations/expenses, Research Funding; Takeda: Consultancy, Honoraria, Research Funding; Amgen: Consultancy, Honoraria, Research Funding; Bristol-Myers Squibb: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding. Klisovic:Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees. Langston:Bristol Myers Squib: Research Funding; Incyte: Research Funding; Jazz Pharmaceuticals: Research Funding; Astellas Pharmaceuticals: Research Funding; Kadmon Corporation: Research Funding; Takeda: Research Funding; Chimerix: Research Funding. Cohen:Janssen, Adicet, Astra Zeneca, Genentech, Aptitude Health, Cellectar, Kite/Gilead, Loxo: Consultancy; Genentech, BMS, Novartis, LAM, BioInvent, LRF, ASH, Astra Zeneca, Seattle Genetics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal